Medical Malpractice Risk Factors: An Economic Perspective of Closed Claims Experience
Vozikis A, Riga M, Pollalis Y
DOI10.21767/2471-9927.100012
1Laboratory of Health Economics and Management, University of Piraeus, Greece
2University of Piraeus, Greece
- *Corresponding Author:
- Vozikis A
Laboratory of Health Economics and Management
University of Piraeus, Piraeus, Greece
Tel: +302104142280
E-mail: avozik@unipi.gr
Received Date: September 05, 2016; Accepted Date: September 24, 2016; Published Date: September 30, 2016
Citation: Vozikis A. Medical Malpractice Risk Factors: An Economic Perspective of Closed Claims Experience. J Health Med Econ. 2016, 2:12.
Copyright: © 2016 Vozikis A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Context: Recent research in Europe and the USA revealed that the number of patients who have experienced a medical error in healthcare has increased worryingly since the last decade, while over half of harm refers to medical errors reasonably preventable. At the same time, surveys indicate that medical errors constitute a significant financial burden on Health Care Systems.
Objectives: The aim of this paper is to present the current situation regarding the medical errors in Greece and to identify the underlying factor contributing to their presence.
Method: We performed an extensive analysis of 287 cases of medical malpractice presented in front of the Greek courts over the last 15 years. The research process included a detailed review of the case while economic and other data where recorded. Then simple descriptive statistical analysis, cross-tabs analysis, ANOVA and logistic regression analysis was applied to unveil information relevant to our research.
Results: The findings from our analysis showed that some 45% of medical errors occur during treatment while most incidents of medical error related to death (37%) or permanent disability (36%). Further, the analysis unveiled that on top of the list of specialties who are involved in cases of medical errors and with higher awarded compensation are those of General Surgery and Obstetrics - Gynecology. In Greece, unlike other countries in the world, the assessment of an overall burden of medical errors is not achievable, mainly due to the absence of any medical error reporting system.
Keywords
Medical errors; Healthcare costs; Patient safety; Health care quality
Introduction
For several years, medical errors are a very common phenomenon, in worldwide which can cause temporary or permanent harm to patients when receiving healthcare. At the same time, the economic burden on the Health Care Systems seems to be very high [1].
The Quality Interagency Coordination Task Force [2] presents the definition for medical error, as follows: “An error is defined as the failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim. Errors can include problems in practice, products, procedures, and Systems”.
In To Err is Human, the IOM [3] sets the definition for an adverse event, as follows: “An adverse event is defined as an injury caused by medical management rather than by the underlying disease or condition of the patient”.
In U.S.A., 98,000 deaths occur annually in hospital care due to medical errors [4] and in U.K. between 20,000 to 30,000 patients die each year, as a consequence of adverse events while a greater proportion of patients is suffered by health complications [5,6]. In Germany, 30,000 patients die every year [4] and in New Zealand, over 50,000 hospitalized patients have harmed by one or more medical errors [7]. In Greece, there are no official statistics for the current situation regarding the medical errors due to an absence of any medical error reporting system which obstructs any attempt of recording and analysis of adverse events and medical errors in Greece. The detection of adverse events and medical errors is through spontaneous reporting and thus finally identified, only a small number of them [1]. However, informal Greek statistics mention that between 20 to 30 patients die every day and about 200 patients daily suffer from serious medical errors, many of which could have been prevented [8].
The aim of this paper is to present the current situation regarding the medical errors in Greece through Greek courts’ judgments and also to display the main characteristics of Medical Error Reporting Information System (MERIS) which used to identify, collect, report and analyze medical errors and patient adverse events, for enhancing the patient safety and health care quality.
Materials and Methods
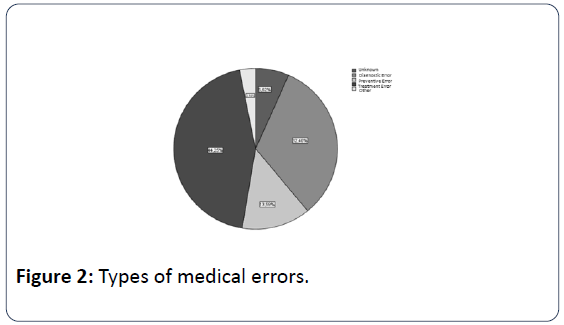
Our research was conducted through Greek courts’ judgments with a sample of 287 cases, associated with medical malpractice, over the last 10 years. The research process includes a detailed overview of the content of legal cases and the establishment of a database that records encoded data related to (e.g.): (a) Type of Health Care Unit, (b) Medical Specialty, (c) Description of case, (d) Phase of care, (e) Severity of Medical Error, (f) Amount of financial compensation. Following, the classification of medical errors’ types, deals with [9]:
Treatment Errors
Preventive Errors
Other
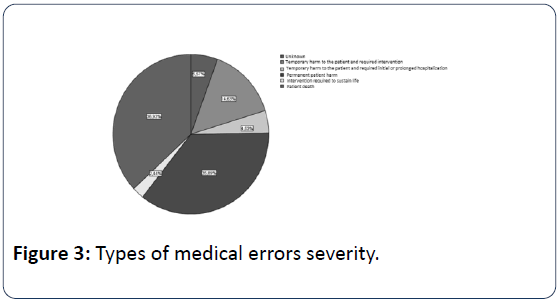
The National Coordinating Council for Medication Error Reporting and Prevention [10] displays the following categories of severity, in case medical errors do cause harm:
Category E (Temporary harm to the patient and required intervention)
Category F (Temporary harm to the patient and required initial or prolonged hospitalization)
Category G (Permanent patient harm)
Category H (Intervention required to sustain life)
Category I (Patient death)
Then, simple descriptive statistical analysis, cross-tabs analysis, ANOVA and logistic regression analysis was applied to unveil information relevant to our survey.
Results
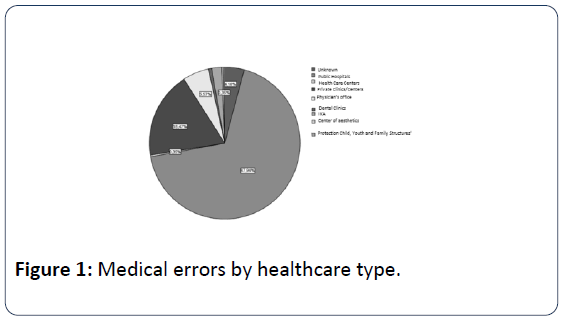
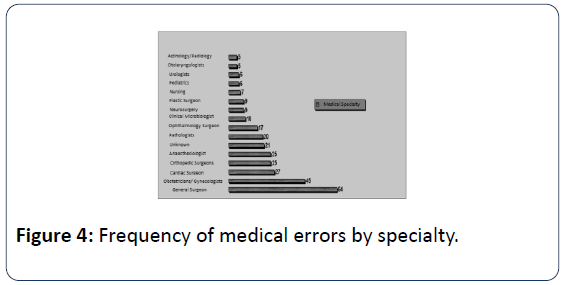
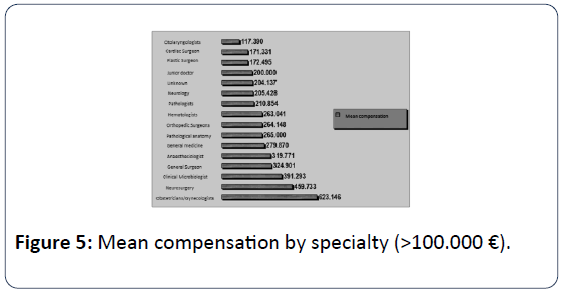
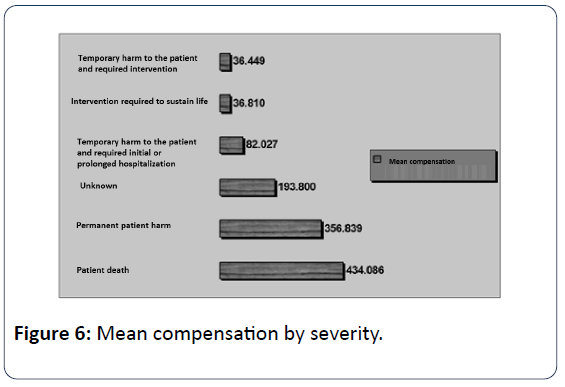
In public hospitals seem to occur more medical errors (67.94%) than in private health sector, but this is normally due to the fact that a large proportion of sample coming from Administrative Courts (Figure 1). Most medical errors happen during the Treatment with 44.25%, followed by errors at phase of Diagnosis with 32.40% (Figure 2). The 36.93% of medical errors resulted in death and 35.89% permanent disability (Figure 3). The interventional specialties of Obstetrics and Gynecology and General Surgery gather more incidents of medical errors (Figure 4). The "responsible" medical specialties for the highest financial compensations are again all surgical specialties and follow Anesthesiologists (Figure 5). The highest mean compensation awarded by courts in patient death (Figure 6).
According to preliminary newer findings from the analysis of 680 cases of awarded compensations, we applied a logistic regression model for the modelling of the medical errors’ severity contributing factors.
So, we set two levels of medical errors severity:
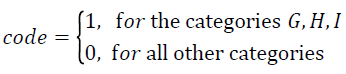
We modelled the probability p of the onset of medical error of high severity (meaning any medical error falling in the categories G, H, I). Using the variables analysis as in Table 1, we incorporated in the regression equation the variables Specialty, Type of Medical Error, ICD-10 Code and Type of Care (Pathological or Surgical), that are statistically significant.
Table 1: Variables in the model.
| B | S.E. | Wald | df | Sig. | Exp(B) | |
|---|---|---|---|---|---|---|
| TYPE OF MEDICAL ERROR | 0,96 | 4 | 0,916 | |||
| TYPE OF MEDICAL ERROR(1) | -154,453 | 16986,046 | 0 | 1 | 0,993 | 0 |
| TYPE OF MEDICAL ERROR(2) | -17,233 | 15209,012 | 0 | 1 | 0,999 | 0 |
| TYPE OF MEDICAL ERROR(3) | -47,317 | 15438,361 | 0 | 1 | 0,998 | 0 |
| TYPE OF MEDICAL ERROR(4) | -16,357 | 15209,012 | 0 | 1 | 0,999 | 0 |
| SPECIALTY | 1,616 | 28 | 1 | |||
| SPECIALTY(1) | -89,666 | 100485,099 | 0 | 1 | 0,999 | 0 |
| SPECIALTY(2) | -17,679 | 94033,124 | 0 | 1 | 1 | 0 |
| SPECIALTY(3) | -64,452 | 114852,129 | 0 | 1 | 1 | 0 |
| SPECIALTY(4) | 8,928 | 93459,776 | 0 | 1 | 1 | 7537,217 |
| SPECIALTY(5) | 47,841 | 101851,942 | 0 | 1 | 1 | 5,99E+20 |
| SPECIALTY(6) | -11,655 | 93626,129 | 0 | 1 | 1 | 0 |
| SPECIALTY(7) | -45,896 | 94060,1 | 0 | 1 | 1 | 0 |
| SPECIALTY(8) | -42,034 | 105107,382 | 0 | 1 | 1 | 0 |
| SPECIALTY(9) | -0,894 | 74601,08 | 0 | 1 | 1 | 0,409 |
| SPECIALTY(10) | 23,896 | 93611,82 | 0 | 1 | 1 | 2,39E+10 |
| SPECIALTY(11) | 7,103 | 93459,776 | 0 | 1 | 1 | 1216,187 |
| SPECIALTY(12) | -47,369 | 145681,831 | 0 | 1 | 1 | 0 |
| SPECIALTY(13) | -12,866 | 93709,058 | 0 | 1 | 1 | 0 |
| SPECIALTY(14) | -85,166 | 102488,278 | 0 | 1 | 0,999 | 0 |
| SPECIALTY(15) | -14,124 | 101735,951 | 0 | 1 | 1 | 0 |
| SPECIALTY(16) | -68,359 | 93546,736 | 0 | 1 | 0,999 | 0 |
| SPECIALTY(17) | -53,258 | 93513,278 | 0 | 1 | 1 | 0 |
| SPECIALTY(18) | 25,47 | 94095,863 | 0 | 1 | 1 | 1,15E+11 |
| SPECIALTY(19) | 86,476 | 102298,712 | 0 | 1 | 0,999 | 3,60E+37 |
| SPECIALTY(20) | 27,337 | 99472,535 | 0 | 1 | 1 | 7,46E+11 |
| SPECIALTY(21) | 5,881 | 93459,776 | 0 | 1 | 1 | 358,151 |
| SPECIALTY(22) | 26,522 | 95264,807 | 0 | 1 | 1 | 3,30E+11 |
| SPECIALTY(23) | -48,714 | 93846,831 | 0 | 1 | 1 | 0 |
| SPECIALTY(24) | 42,981 | 133561,607 | 0 | 1 | 1 | 4,64E+18 |
| SPECIALTY(25) | 90,001 | 116007,584 | 0 | 1 | 0,999 | 1,22E+39 |
| SPECIALTY(26) | 42,166 | 273394,117 | 0 | 1 | 1 | 2,05E+18 |
| SPECIALTY(27) | -31,968 | 67506,37 | 0 | 1 | 1 | 0 |
| SPECIALTY(28) | 26,533 | 94157,902 | 0 | 1 | 1 | 3,34E+11 |
| ICD-10 CODE | 1,151 | 19 | 1 | |||
| ICD-10 CODE(1) | 38,938 | 67489,548 | 0 | 1 | 1 | 8,14E+16 |
| ICD-10 CODE(2) | 3,526 | 55112,097 | 0 | 1 | 1 | 33,979 |
| ICD-10 CODE(3) | 150,086 | 69711,942 | 0 | 1 | 0,998 | 1,52E+65 |
| ICD-10 CODE(4) | -31,688 | 55452,663 | 0 | 1 | 1 | 0 |
| ICD-10 CODE(5) | -18,009 | 88637,218 | 0 | 1 | 1 | 0 |
| ICD-10 CODE(6) | 37,221 | 60906,558 | 0 | 1 | 1 | 1,46E+16 |
| ICD-10 CODE(7) | -11,57 | 68487,018 | 0 | 1 | 1 | 0 |
| ICD-10 CODE(8) | -33,358 | 55452,663 | 0 | 1 | 1 | 0 |
| ICD-10 CODE(9) | 42,16 | 55473,917 | 0 | 1 | 0,999 | 2,04E+18 |
| ICD-10 CODE(10) | -32,669 | 55452,663 | 0 | 1 | 1 | 0 |
| ICD-10 CODE(11) | 0,937 | 55883,802 | 0 | 1 | 1 | 2,551 |
| ICD-10 CODE(12) | 37,071 | 56629,548 | 0 | 1 | 0,999 | 1,26E+16 |
| ICD-10 CODE(13) | 44,805 | 67803,266 | 0 | 1 | 0,999 | 2,88E+19 |
| ICD-10 CODE(14) | 24,724 | 54766,301 | 0 | 1 | 1 | 5,46E+10 |
| ICD-10 CODE(15) | -29,658 | 60820,429 | 0 | 1 | 1 | 0 |
| ICD-10 CODE(16) | -31,927 | 74588,272 | 0 | 1 | 1 | 0 |
| ICD-10 CODE(17) | -33,858 | 55452,663 | 0 | 1 | 1 | 0 |
| ICD-10 CODE(18) | 1,795 | 55331,554 | 0 | 1 | 1 | 6,02 |
| ICD-10 CODE(19) | 59,787 | 56282,973 | 0 | 1 | 0,999 | 9,23E+25 |
| TYPE OF CARE(1) | 44,173 | 3173,311 | 0 | 1 | 0,989 | 1,53E+19 |
| Constant | 43,249 | 107589,67 | 0 | 1 | 1 | 6,07E+18 |
a. Variable(s) entered on step 1: TYPE OF MEDICAL ERROR.
b. Variable(s) entered on step 2: ICD-10 CODE.
c. Variable(s) entered on step 3: TYPE OF CARE.
d. Variable(s) entered on step 4: SPECIALTY.
The predictive function incorporates the 4 contributing variables (factors) and estimates the probability p. More specifically, we have:
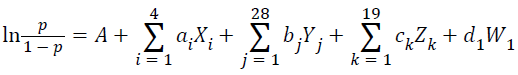
Where,
• A=43, 249
• The Xi, i=1,2,3,4 are indicative variables, referring to the contributing factor TYPE OF MEDICAL ERROR
• The Yj, j=1,2,…,28 are indicative variables, referring to the contributing factor SPECIALTY
• The Zk, k=1,2,…,19 are indicative variables, referring to the contributing factor ICD-10 CODE
• The W refers to the contributing factor TYPE OF CARE
The medical error severity seems also to be statistically significant for the awarded compensation amount (Table 2).
Table 2: Test of between-subjects effects.
| Tests of Between-Subjects Effects Dependent Variable: Awarded Compensation Amount |
|||||
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Corrected Model | 8,496E12 | 6 | 1,416E12 | 5,071 | 0,000 |
| Intercept | 2,331E12 | 1 | 2,331E12 | 8,348 | 0,004 |
| Medical Error Severity | 8,496E12 | 6 | 1,416E12 | 5,071 | 0,000 |
| Error | 5,892E13 | 211 | 2,792E11 | ||
| Total | 8,712E13 | 218 | |||
| Corrected Total | 6,741E13 | 217 | |||
| a, R Squared = 0,126 (Adjusted R Squared = 0,101) | |||||
Moreover (as shown in Table 3) the higher awarded compensation amounts are related to the severity categories I and G.
Table 3: Estimates test of between-subjects effects.
| 95% Confidence Interval | ||||
| Medical error severity | Mean | Std, Error | Lower Bound | Upper Bound |
| 9176,905 | 115310,078 | -218130,467 | 236484,277 | |
| Unknown | 177649,787 | 152540,895 | -123049,602 | 478349,176 |
| Category E | 42927,524 | 90622,796 | -135714,533 | 221569,580 |
| Category F | 152265,487 | 176139,054 | -194952,260 | 499483,233 |
| Category G | 333195,515 | 59831,462 | 215251,511 | 451139,519 |
| Category H | 98938,000 | 373647,358 | -637622,069 | 835498,069 |
| Category I | 551762,133 | 67109,047 | 419472,039 | 684052,227 |
Discussion and Practical Implications
Our research findings are consistent and agree with the findings of other surveys, according to the literature [11]. In a survey of USA the specialties of General Surgery and Obstetrics and Gynecology occurred in the first two positions as responsible for causing harm due to medical malpractice [12]. Same findings for Greece are presented by other similar research studies [13,14].
In the very recent 2016 Medical Malpractice Annual Report, General Surgery and Obstetrics and Gynecology are the physician specialties that had the largest number of claims with paid indemnity, while Pediatrics and Obstetrics and gynecology had the higher Median paid indemnity [15].
In a similar study, among medical specialties, obstetricians were again involved in the most cases, as well as the highest total and average awards followed by Anesthesiologists [16].
In another study, the results highlight the frequency and severity problems plaguing the Obstetrics and Gynecology specialty. Higher frequencies and severities are also seen in neurosurgery, while neurology – invasive shows a high severity but a low frequency [17]. These, results to the malpractice insurance fees for obstetricians are set to increase. The major hike in fees is directly related to the number of claims and level of awards by the courts in cases taken by parents, mainly over brain damaged babies [18].
At this point, it should be clarified that medical errors and adverse events mainly occurred as a consequence of systemic problems in a healthcare [1]. In specific, the medical understaffing in hospitals, the unsafe working environment, the severity of the patients’ disease, the increased workload, the circular time, the inadequate staff in nursing and the burnout of health professionals, are the most important root causes of medical errors. Especially in Greece, as economic crisis has caused dramatic significant budget cuts in the financing of the National Health System for years, health indicators may not have a rapid recovery and thus public health may be a real “chronic patient” [19].
This is more obvious, taking in consideration the strong positive association between low patient satisfaction level in Greece and healthcare provision indicators that are worsening in the last 7 years [20].
So as an added value policy proposal, the MERIS, a blamefree system, implemented in a protected environment that encourages the systematic recording and reporting of adverse events and medical errors, may contribute to enrich the knowledge for the contributing factors of medical errors [21].
Some basic recommendations for a successful reporting system, may incorporate the following characteristics:
• Building stakeholders’ awareness of medical errors
• Mapping out a national-wide strategy with the usage of Health Information Technology
• Promoting quality assurance practices, patient safety standards and decision making process in reducing the adverse events and medical errors
• Educating health professionals and patients in patient safety reporting system
To sum up, this paper has not at all the tension to blame any health professionals, but only to raise the awareness to all stakeholders for taking preventive actions for reducing medical errors and adverse events.
Acknowledgment
Part of the work had been presented at 2nd International Symposium and 24th National Conference on Operational Research, 26-28 September, 2013, Athens, Greece.
References
- Vozikis A, Riga M (2012) Patterns of medical errors: A challenge for quality assurance in the Greek Health System. In: Savsar M (ed.) Quality Assurance and Management. pp:245-266.
- Quality Interagency Coordination Task Force (2000) Doing what counts for patient safety: federal actions to reduce medical errors and their impact.
- Institute of Medicine (1999) To Err is human: building a safer health system. Washington DC, National Academy Press.
- McLean (1997) Nationwide poll on patient safety: 100 million Americans see medical mistakes directly touching them. VA: National Patient Safety Foundation.
- Starfield B (2000) Is US Health Really the Best in the World? JAMA 284:483-485.
- Thomas EJ, Studdert DM, Runciman WB, Webb RK, Sexton EJ, et al. (2000) A comparison of iatrogenic injury studies in Australia and the USA, I: Context, methods, casemix, population, patient and hospital characteristics. Int J Qual Health Care 12: 371–378.
- Bismark M, Dauer E, Paterson R, Studdert D (2006) Accountability sought by patients following adverse events from medical care: the New Zealand experience-Research. Can Med Assoc J 175: 889-894.
- Vozikis A, Riga M (2008) Medical errors in Greece: The economic perspective through the awards of administrative courts. Society Economy and Health 2: 22-44.
- Leape LL (1993) Preventing Medical Injury. QRB Qual Rev Bull 19:144-149.
- National Coordinating Council on Medication Error Reporting and Prevention (1998). Taxonomy of medication errors.
- Pollalis Y, Vozikis A, Riga M (2012) Qualitative patterns of medical errors: research findings from Greece. Rostrum of Asclepius 11:577-592.
- U.S. Department of Health and Human Services (2002) Confronting the new health care crisis: improving health care quality and lowering costs by fixing our medical liability system. Washington, DC.
- Riga M, Vozikis A, Pollalis Y, Souliotis K (2015) MERIS (Medical Error Reporting Information System) as an innovative patient safety intervention: A health policy perspective. Health Policy 119:539–548.
- Riga M, Vozikis A, Pollalis Y (2014) Medical errors in Greece: an economic analysis of compensations awarded by civil courts (2000-2009). Open Journal of Applied Sciences 4:168-175.
- Office of the Insurance Commissioner (2016) Medical Malpractice Annual Report. WA, OIC.
- The Risk Authority Stanford (2015) Medical malpractice trend review. Stanford University Medical Network, CA.
- Pinnacle Actuarial Resources, Inc. (2004) Oregon professional panel for analysis of medical professional liability insurance: a report on factors impacting medical malpractice insurance availability and affordability. Pinnacle Actuarial Resources, Inc., Bloomington.
- Irish Health analysis (2016) Malpractice crisis hits obstetrics. Dublin, Ireland.
- Vozikis A, Xesfingi S(2016) Patients’ satisfaction with the health care system: Assessing the impact of socio-economic and health care provision factors. BMC Health Services Research 16:94.
- Fragoulakis V, Athanasiadi E, Mourtzikou A, Stamouli M, Vozikis A(2014) The health outcomes in recession: preliminarily Findings for Greece. International Journal of Reliable and Quality E-Healthcare 3:55-65.
- Vozikis A (2009) Information management of medical errors in Greece: The MERIS Proposal. Int J Inf Manage 29:15–26.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences