Improving Health Care System Efficiency for Equity, Quality and Access: Does the Healthcare Decision Making Involve the Concerns of Equity? Explanatory Review
Mende Mensa Sorato*, Akbar Abdollahi Asl and Majid Davari
DOI10.36648/2471-9927.6.1.45
Mende Mensa Sorato*, Akbar Abdollahi Asl and Majid Davari
Department of Pharmacoeconomics and Pharmaceutical Administration, Faculty of Pharmacy, Tehran University of Medical Sciences, Iran
- *Corresponding Author:
- Mende Mensa Sorato
Department of Pharmacoeconomics and Pharmaceutical Administration
Faculty of Pharmacy, Tehran University of Medical Sciences, Iran
Tel: +98-9056309138
E-mail: mendemensa123@gmail.com
Received Date: April 06, 2020; Accepted Date: May 12, 2020; Published Date: May 19, 2020
Citation: Sorato MM, Asl AA, Davari M (2020) Improving Health Care System Efficiency for Equity, Quality and Access: Does the Healthcare Decision Making Involve the Concerns of Equity? Explanatory Review. J Health Med Econ. Vol. 6 No. 1: 45.
DOI: 10.36648/2471-9927.6.1.45
Abstract
Background: Healthcare is a complex investment which requires a number of stakeholders to produce desired health outcomes. In addition to its complex nature, availability of limited resources for providing healthcare for population poses a number of questions for policy makers. Among these multitudes of questions, Efficiency, Equity and Effectiveness have complex interplay and require balanced tradeoff. Therefore, this explanatory review was conducted with intention to provide basic information on how to incorporate efficiency, equity and effectiveness in healthcare decision making.
Method: We systematically searched PubMed/Medline, Scopus, and Google scholar with the following with the following queries: Effectiveness, Efficiency, Equity, Delivery of healthcare, Health care decision making.
Results: Inefficiency in health systems is a global problem. About 20-40% global health expenditure is considered as w stage. Efficiency, Effectiveness and Equity are synergistic pillars of quality healthcare system. Improving efficiency in health system can reduce raising healthcare expenditure. Providing equitable care for all has national and international importance. Priority setting, multiple criteria decision making and incorporation of equity impact and trade-off analysis on costeffectiveness can be used for balancing tradeoff between efficiency, equity and effectiveness.
Conclusion: Efficiency of healthcare system is important for improving, equity, effectiveness and access to healthcare. Taking efficiency into healthcare delivery with full understanding of determinants of disease in specific population can provide room for improving effectiveness and equity in healthcare as evidenced by presence of avoidable wastages and inefficiency in every healthcare system. Equity should be considered during planning process along with economic evaluations.
Keywords
Efficiency; Equity; Effectiveness; Healthcare decision making
Introduction
Healthcare is a complex investment which requires a number of stakeholders (direct and indirect) contribution to produce the desired health outcomes. In addition to its complex nature imperfect market in the field and limited/scarce resources for providing healthcare for population poses a number of questions for policy makers. Among these multitudes of questions, Efficiency, Equity and Effectiveness have complex interplay and require balanced tradeoff between them [1].
Efficiency is a measure of the quality and/or quantity of output for a given level of input. It could be technical or allocative. Allocative Efficiency is use of limited resources towards producing the correct mix of health care outputs. Technical Efficiency is the extent to which the system is minimizing its inputs in producing its chosen outputs, regardless of the value placed on those outputs [1-3].
Inefficiency in health systems is a global problem and approximately 20-40% of all resources spent on health were wastage [1]. For example, $760 billion to $935 billion, accounting for approximately 25% of total health care spending in US health system is wastage [4]. In Namibia 52% Public Hospitals were technically inefficient [5]. In Ghana only 24% district hospitals were technically efficient [6]. In Eretria about 68% of hospitals were technically efficient and only 42% were scale efficient [7]. Similar study conducted in 2016 among primary health centers in Ethiopia showed that 54% of sampled health centers were technically inefficient [8].
Major reasons for inefficiency in health sector include: in appropriate Medicine use; over or under supply health services; inappropriate Health task force mix, medical errors, suboptimal quality of care, corruption and poor integration of health facilities [1,9]. Today almost all countries in the world are focusing on efficiency of their health care system to ensure universal health coverage [1,2,10-12]
In addition to inefficiency problem, health system is also suffering from equity problem. This is because health economic evaluations continue to focus on maximizing health gain and health equity considerations are rarely mentioned [13].
Health care system should ensure access to: good quality care for patients who need them at a reasonable price. There is always debate on three important terms, efficiency, equity, and Effectiveness. They usually go together and right approach to address them will improve welfare of society [14,15]. Despite the presence evidence about effectiveness is healthcare interventions, translating evidences into practice requires tradeoff between effectiveness, efficiency and equity due to scarcity of available health resources [16]. However, Policy makers and managers in the health care system face difficulty in addressing them together. This explanatory review was conducted with intension to describe the role of addressing efficiency on equity, effectiveness and access to healthcare.
Methods
Search strategy
We have systematically searched PubMed/Medline, Scopus, and Google scholar with the following with the following search query. Effectiveness, Efficiency, Equity, Delivery of healthcare, Health care decision making.
Inclusion exclusion criteria
• Studies described Efficiency, equity, effectiveness and healthcare decision making were included
• Studies conducted in English Language are included
• Short communications, and conference proceedings are excluded
Study selection and Evidence synthesis
From total of 152 articles identified by literature search 93 potentially relevant articles were selected, after applying the inclusion exclusion criteria listed above only 65 articles were found to be relevant [17] (Figure 1). Two investigators (MM, AA) independently reviewed each study’s abstract against prespecified inclusion and exclusion criteria. In case of disagreement on quality of the article two authors discussed In front of table in presence of the third author (MD).
Evidence synthesis
We qualitatively synthesized the evidence. Firstly we defined efficiency how to measure efficiency in Healthcare system.
Secondly we answered the following questions. Can efficient systems in inequitable? Can efficient systems improve equity? Can efficient systems improve quality of care? Can efficient systems improve access to care? What is optimum level tradeoff between these variables? How to incorporate them in Healthcare decision making process/Can our Cost-effectiveness evaluation consider the issue of equity?
Results
What is efficiency?
Efficiency can be defined as the ratio of output to the input i.e. (Efficiency = Output/Input). However measuring efficiency organizations with multiple outputs and inputs like hospitals is difficult to determine by the above model. Therefore efficiency of organizations with multiple inputs and outputs can be calculated by weighed cost approach as follows [18,19].
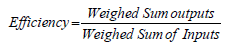
The above equation assumes all the weights are uniform. Mathematically it is expressed as:
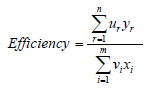
Where: yáµ£=quantity of output r; uáµ£=weight attached to output r; xáµ¢=quantity of input i; váµ¢=weight attached to input i. Value equal to one indicates perfect efficiency (100%) and 0 ≤ Efficiency ≤ 1.
Technical efficiency of an organization can be measured from input orientation or out-put orientation. In the former we pull all the DMUs to origin towards efficiency frontier and the curve takes convex shape (i.e. we require small inputs to produce large outputs to improve efficiency). While in case of output orientation we push all DMUs away from the origin towards the frontier and the curve takes concave shape (i.e. to improve efficiency large outputs should be produced with similar inputs [3,20]. This approach answers the question by how much quantities an output can be expanded without changing the inputs. In this case we push the DMUs away from the origin towards efficiency frontier and the curve takes concave shape. Both output and input orientation will only provide equivalent estimates of technical efficiency if there is constant rate of return scale and they are unequal when decreasing or increasing rate of return exist [21].
Efficiency, equity and effectiveness
The Institute of Medicine defines health care quality as the degree to which health care services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge Quality is defined by the following domains: Effectiveness, Efficiency, Equity, Patient centeredness, Safety and Timeliness of care delivery [22-25].
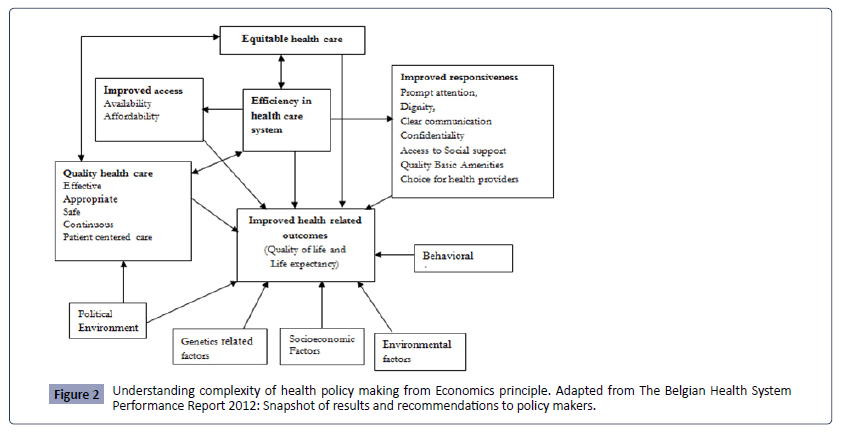
Efficiency, Equity and Effectiveness are core values of quality healthcare (Figure 2). They are interrelated and if appropriately considered they are synergistic in nature. However, if not considered appropriately in healthcare decision making they might result in an adverse outcome [22-27].
How can efficiency improve equity?
Equity is the absence of avoidable or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically. Health inequities therefore, involve more than inequality with respect to health determinants, access to the resources needed to improve and maintain health or health outcomes [28,29].
Health Care Financing in low and middle income countries are pro-rich and there unmet equity needs to unsure universal health coverage. The distribution of benefits at the primary health care level favored the poor while hospital level services benefit the better-off [30]. The richest quintile receives 19.2% of total benefits compared to the 17.9% received by the poorest quintile. The rich also receive a much higher share of benefits relative to their need [24].
Efficiency deals with maximization of outputs or minimization of wastage. Through reduction in wastage, there is potential saving of resources. Since equity requires fair distribution of resources or services among the entire population irrespective of irrelevant factors like race, ethnicity and place of residence, redistribution of the savings generated by efficient utilization of resources will improve the equity [31].
The potential benefits of considering equity are likely to be largest in cases involving: (a) interventions that target disadvantaged individuals or communities and are also relatively cost-ineffective and (b) interventions to encourage lifestyle change, which may be relatively ineffective among ‘hard-to-reach’ disadvantaged groups and hence may require re-design to avoid increasing health inequalities [13].
If Equity is not addressed, the vulnerable population will have low access to services and with inferior quality [32]. In addition to this improving quality of services may requires improving standards, service delivery system or technical capacity of providers these all require financial capacity and improving efficiency can also give room to improve quality of healthcare delivery [31,33,34].
How efficiency improves access to care?
Access to healthcare is also a complex concept and it includes; availability, affordability and acceptability. Access is influenced by distribution of scarce healthcare resources from supply side and individual’s socio-economic status, education, knowledge, cultural beliefs and personal preferences from demand side. Different indicators may be used to measure access to healthcare, such as waiting time for healthcare, availability of resources and cost of access to available service, availability of medical personnel, infrastructure, and equipment, distance, time and cost of travel [15].
Universal access to healthcare in developing countries is not ensured. Many millions of people suffer and die from conditions for which there exist effective interventions. Diseases like diarrhea, pneumonia, and malaria are responsible for 52% of child deaths worldwide. For each disease there is at least one effective prevention and one effective treatment [35]. Poverty is the main barrier to access healthcare access in developing countries which is synergized by inefficient healthcare system [36].
Improving efficiency or reducing wastage leads to saving healthcare budget. This saved money can be spent on less accessible products and/or services. This is particularly important in settings with limited health budget to provide equitable care for their population [1,37-39].
What to sacrifice at what level?
Efficiency, effectiveness and equity have multiple interactions. They affect the core goal of health system (i.e. ensuring access to quality care without casing financial catastrophe). Availability of limited healthcare resources raises question of how should limited health care resources be allocated? What health services should be publicly funded? How should indications for particular interventions be defined? The health system should consider them during setting health care strategies and goals. When the one attempts to make more equitable distribution of healthcare, it may lead to decrease in efficiency. This cost should be considered when trying to improve equity [40,41].
How to incorporate equity in Healthcare decision making process?
The interaction between efficiency and equity needs careful tradeoff as we are living in scarce world where nothing is given as a free lunch. This is because an inefficient allocation can be equitable, an efficient allocation can be inequitable, an inefficient allocation can become more efficient without increasing inequity, what is equitable often requires inequality in health and inequality in resource distribution per capita [42].
Therefore, we prioritize among available alternatives based on disease related, social and financial related factors. Prioritysetting in health care is the task of determining the priority to be assigned to a service, a service development or an individual patient at a given point in time. Prioritization is needed because claims (whether needs or demands) on healthcare resources are greater than the resources available [43]. Explicitly addressing priority setting is necessary to develop fairer methods of allocation for scarce health care resources and to begin a public dialogue to ensure legitimacy in the process [44].
Generally, we have two methods of priority setting; non-economic and economic methods. The non-economic method involves; historical allocation and intensities; needs assessment, burden of disease, cost-of-illness and Defining core services. Economic method involves Pharmacoeconomic evaluations [45,46].
Cost effectiveness analysis (CEA) can address concerns of health equity if; equity impact analysis, which quantifies the distribution of costs and effects by equity stratifying variables and equity tradeoff analysis, which quantifies trade-offs between improving total health and other equity objectives were included [47]. In addition to this, integration of distributional concerns through equity weights and social welfare functions, exploration of the opportunity costs of alternative policy options through mathematical programming, and multi-criteria decision analysis can also help to address equity concerns in economic evaluation [48].
Guidance for Priority Setting (GPS) in Health Care, initiated by WHO, offers a comprehensive map of equity criteria that are relevant to health care priority setting and should be considered in addition to cost-effectiveness analysis. The GPS-Health incorporates criteria related to the disease an intervention target; characteristics of social groups an intervention and non-health consequences of an intervention (financial protection, economic productivity, and care for others) [49] (Table 1).
Table 1 Priority-setting criteria to be considered in conjunction with cost-effectiveness results.
| Criteria | Question | Weight given |
|---|---|---|
| Group 1: | Disease and intervention criteria | |
| Severity | Have you considered whether the intervention has special value because of the severity of the health condition (present and future health gap) that the intervention targets? | |
| Realization of potential | Have you considered whether the intervention has more value than the effect size alone suggests on the grounds that it does the best possible for a patient group for whom restoration to full health is not possible? | |
| Past health loss | Have you considered whether the intervention has special value because it targets a group that has suffered significant past health loss (e.g. chronic disability) | |
| Group 2: | Criteria related to characteristics of social groups | |
| Socioeconomic status | Have you considered whether the intervention has special value because it can reduce disparities in health associated with unfair inequalities in wealth, income or level of education? | |
| Area of living | Have you considered whether the intervention has special value because it can reduce disparities in health associated with area of living? | |
| Gender | Have you considered whether the intervention will reduce disparities in health associated with gender? | |
| Race, ethnicity, religion and sexual orientation | Have you considered whether the intervention may disproportionally affect groups characterized by race, ethnicity, religion, and sexual orientation? | |
| Group 3: | Criteria related to protection against the financial and social effects of ill health | |
| Economic productivity | Have you considered whether the intervention has special value because it enhances welfare to the individual and society by protecting the target population’s productivity? | |
| Care for others | Have you considered whether the intervention has special value because it enhances welfare by protecting the target population’s ability to take care of others? | |
| Catastrophic health expenditures | Have you considered whether the intervention has special value because it reduces catastrophic health expenditures for the target population? |
Since efficiency, equity and financial protection are considerations that sometimes conflict with each other, decision makers need to weigh them against each other and make trade-offs. It should be recognized that, in a resource-constrained system, giving additional weight to something or someone implies that something or someone else will lose out. The inclusion of equity concerns must therefore always take opportunity costs into consideration [49,50].
Another method to consider priority setting criteria for selecting health interventions/technologies is using multi-criteria approach for appropriate decision making [51]. Multiple criteria decision making is a process involving, multiple alternatives containing multiple criteria evaluated by multiple evaluators to produce common result. Steps in a Multiple Criteria Decision Analysis (MCDA) include: Define the context, Identify the options available, decide the objectives and select the right criteria that represent the value, Measure out each of the criteria in order to discern their relative importance and calculate the different values by averaging out weighting and scores [52].
Discussion
This min review we have included 65 articles for evidence synthesis. The review revealed the interaction core measures of quality health system (efficiency, equity and effectiveness). We answered the following questions: Can efficient systems be inequitable? Can efficient systems improve equity? Can efficient systems improve quality of care? Can efficient systems improve access to care? What is optimum level tradeoff between these variables? And how to incorporate equity in Healthcare decision making process?
Availability of limited resources for healthcare, diversity of unmet health needs and external influence of variables outside the healthcare system on health mandates the policy makers and health economists to tradeoff between efficiency, equity and effectiveness [40,41]. These variables mean different for different sectors, patients, hospitals, insurance companies and health system as whole. Patients need quality and evidencebased care and Hospitals want to provide evidence-based care for their patients to maintain their credibility and continue in business. However, insurance companies want to provide efficient healthcare to managed costs and continue in investment. Above all health system and political system proclaim to the society that they are providing quality Up-to-date care and wants to achieve excellence in healthcare for next election [53].
Efficiency is the question of every healthcare system in the world. This is because there is significant avoidable wastage in resource utilization or technical allocation [1]. For example, failures of care delivery; failures of care coordination; overtreatment; administrative complexity; price failures; and fraud and abuse are identified areas of wastage. Addressing them could produce gains of at least 20% of total health care expenditures [54-56].
Today almost all countries in the world are facing budget constraint in health spending, which force them focus on efficiency of their health care system to ensure universal health coverage. However according to WHO Report 20–40% of all resources spent on health were wastage [1,10-12]. Integrated care which can avoid unnecessary duplication, improving working flow, using improved health records, improving governance structure and transparency will help to improve efficiency system [57-61]. This is in line with reasons of inefficiency; inappropriate use of medicines, inappropriate allocation of Health-care resources and services and leaking Health system which provide room for corruption and fraud [1].
Three Es’ (efficacy, equity and effectiveness) are interrelated and if appropriately considered they are synergistic in nature [62]. However, if not considered appropriately in healthcare decision making they might result in adverse outcome. For example, if the health system ignores the small segment of socially disadvantaged groups and focus on the majority of the population, adverse outcomes among socially disadvantaged group due to lack of basic healthcare will disturb the entire society. The effects may be in the form of migration, crime and diseases (e.g. infectious diseases or antimicrobial resistance) [22-25].
Considering efficiency in health care system, can provide room for improving, equity, quality, and access of healthcare by directly or indirectly. Assume that recommendation is input minimization to provide desired healthcare services based on input-orientation. The resource retained/saved by this approach can be refunded for improving equity of care by establishing new institutions or training additional health task forces. Availability of additional resource may also allow the system to improve quality standards of the service delivery through accreditation and application of guidelines and standards of evidence-based care. Being efficient in healthcare system means more than saving money or reducing wastage [63].
Due to scarcity healthcare resources tradeoff between efficiency, equity and effectiveness is important during healthcare decision making. The question here is what to tradeoff and by how much? This is probably the most difficult question researchers and policy makers may face during selecting health interventions. There is no clear-cut point for the tradeoff, but the following options can be applied: Priority setting and multi-criteria decision making [64-67]. During prioritization policy makers should consider the following domains: intervention outcomes and Benefits, type of health service, disease impact (burden), therapeutic context, economic impact, environmental impact of the intervention, quality/uncertainty of evidence, implementation complexity, priorities (fairness) and Overall Context [68].
Ensuring efficiency in health care system can give room for quality improvement. Quality is defined by different countries differently depending on availability of resources and technology. It is achieving the highest possible degree of excellence in health care. Achieving this level cannot be simple for most countries in the world due technical or financial limitations [69]. Working on efficiency of the healthcare system can help to save money. Through this efficiency can contribute to quality of healthcare delivery [70].
Equity in healthcare delivery is avoiding non-justifiable barriers to essential healthcare like, race, ethnicity and wealth status. Providing equitable care for all has national and international importance [71,72]. This is because consequence of the disease in the specific marginalized population could be beyond the boarder of that population. A good example are, Ebola epidemic in Democratic Republic of Congo, Corona Virus in Wuhan city. In addition to this inequitable healthcare could have further economic decline, unemployment, crime and social instability [73,74]. Therefore, balancing efficiency and equity by considering: effectiveness of the program, budgetary impact, reducing inequalities between groups, number of beneficiaries from intervention, ability to access the intervention, cost-effectiveness and quality of the available evidence among particular society is important [68].
Conclusion
In General Efficiency of healthcare system is important for improving, equity, effectiveness and access healthcare for society. Efficiency and equity do not inherently conflict, an inefficient allocation can be equitable and an efficient allocation can be inequitable. Efficiency should be handled carefully because it can improve and deter the healthcare outcomes. Limited availability resources for healthcare, diversity of unmet health needs and external influence of variables outside the healthcare system on health mandates the policy makers and health economists to tradeoff between these variables. Taking efficiency into healthcare delivery with full understanding of determinants of disease in specific population can provide room for improving effectiveness, and equity in healthcare as evidenced by presence of avoidable wastages and inefficiency in every healthcare system. Equity should be considered during the planning process along with economic evaluations. Priority setting or multi-criteria decision making process can used for consideration of equity.
References
- Evans DCaDB (2010) Improving health system efficiency as a means of moving towards universal coverage. World health report 2010 background paper 28.
- Jonathan Cylus IPaPCS (2016) Health system efficiency: How to make measurement matter for policy and management. European Health Observatory. Health policy series 46.
- Timothy J. Coelli DSPR, Christopher J. O'Donnell, George Edward Battese (2005) An introduction to efficiency and productivity analysis.
- Shrank WH, Rogstad TL, Parekh N (2019) Waste in the US Health Care System: Estimated Costs and Potential for Savings.
- Jones CA (2018) Analyzing the Technical Efficiency of Public Hospitals in Namibia. Bethesda, MD: Health Finance and Governance Project, Abt Associates Inc.
- Caroline Jehu-Appiah SS, Adjuik M, Akazili J, Almeida SD, Nyonator F, et al. (2014) Ownership and Technical efficiency of Hospitals: Evidence from Ghana Using Data Envelopment Analysis. Cost Effectiveness and Resource Allocation 12.
- Asbu. JMKaEZ (2013) Technical and scale efficiency of public community hospitals in Eretria: An explanatory study: BMC Health Economics Review 3.
- Mann C DE, Adugna M, and Berman P (2016) Measuring efficiency of public health centers in Ethiopia. Harvard T.H. Chan School of Public Health and Federal Democratic Republic of Ethiopia Ministry of Health. Boston, Massachusetts and Addis Ababa.
- Word Health Organization (2010) National Health Accounts.
- Varabyova Y SJ (2010) International comparisons of the TE of the hospital sector: panel data analysis of OECD countries using parametric and non-parametric approaches. Health Policy 112: 70-9.
- Development. OfEC-oa (2010) Value for money in health spending.
- Winnie Yip RH (2018) Improving Health System Efficiency: Reforms for improving the efficiency of health systems: lessons from 10 country cases.
- Cookson R, Drummond M, Weatherly H (2009) Explicit incorporation of equity considerations into economic evaluation of public health interventions. Health Economics, Policy and Law 4: 231-45.
- Lee TH, Kim W, Shin J, Park EC, Park S (2018) Strategic Distributional Cost-Effectiveness Analysis for Improving National Cancer Screening Uptake in Cervical Cancer: A Focus on Regional Inequality in South Korea. Cancer research and treatment : official j Korean Cancer Association 50: 212-21.
- Cerovic L, Samarà ¾ija N, Brki� M (2016) Balancing Between Efficiency and Equity in Publicly Funded Health Systems. International Public Administration Review, Forthcoming.
- Eisenberg JM (2002) Globalize the evidence, localize the decision: evidence-based medicine and international diversity. Health affairs 21: 166-8.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 4: 1.
- Chisholm D ED (2010) Improving health system efficiency as a means of moving towards universal coverage. Background paper for World health report: Health systems financing: the path to universal coverage. Geneva: WHO.
- Young J, Hulme C, Smith A, Buckell J, Godfrey M, et al. Health Services and Delivery Research. Measuring and optimising the efficiency of community hospital inpatient care for older people: the MoCHA mixed-methods study. NIHR Journals Library.
- Smith PC, & Street, A (2005) Measuring the efficiency of public services: the limit of analysis. Journal of Royal Statistical Society 168: 401-17.
- Coelli T (2009) A Guide to DEAP Version 2.1: A Data Envelopment analysis (Computer program). Center of efficiency and productivity analysis.
- Rudiger A (2016) Human Rights and the Political Economy of Universal Health Care: Designing Equitable Financing. Health Hum Rights 18: 67-78.
- Frezza E (2018) Medical Ethics: A Reference Guide for Guaranteeing Principled Care and Quality. New York: Productivity Press.
- Kwesiga B, Ataguba JE, Abewe C, Kizza P, Zikusooka CM (2015) Who pays for and who benefits from health care services in Uganda? BMC health services research 15: 44.
- Rezapour R, Tabrizi JS, Farahbakhsh M, Saadati M, Abdolahi HM (2019) Developing Iranian primary health care quality framework: a national study. BMC public health 19: 911.
- Vrijens F, Renard F, Jonckheer P, Van den Heede K, Desomer A, et al. (2013) The Belgian Health System Performance Report 2012: Snapshot of results and recommendations to policy makers. Health Policy 112: 133-40.
- Aday LA, Begley CE, Lairson DR, Slater CH, Richard AJ, et al. (1999) A framework for assessing the effectiveness, efficiency, and equity of behavioral healthcare. Am J Manag Care 5: 25-43.
- Ndumbe-Eyoh S, Moffatt H (2013) Intersectoral action for health equity: a rapid systematic review. BMC Public Health 13: 1056.
- Torres S, Labonté R, Spitzer DL, Andrew C, Amaratunga C (2014) Improving health equity: the promising role of community health workers in Canada. Healthc Policy. 10: 73-85.
- Asante A, Price J, Hayen A, Jan S, Wiseman V (2016) Equity in Health Care Financing in Low- and Middle-Income Countries: A Systematic Review of Evidence from Studies Using Benefit and Financing Incidence Analyses 11.
- Jehu-Appiah C, Baltussen R, Acquah C, Aikins M, Amah d'Almeida S, et al. (2008) Balancing Equity and Efficiency in Health Priorities in Ghana: The Use of Multicriteria Decision Analysis. Value in Health 11: 1081-7.
- Fleurbaey M, Schokkaert E (2011) Equity in Health and Health Care. Handbook of Health Economics 1003-92.
- Ngalesoni FN, Ruhago GM, Mori AT, Robberstad B, Norheim OF (2016) Equity impact analysis of medical approaches to cardiovascular diseases prevention in Tanzania. Social Science & Medicine 170: 208-17.
- Mills A, Ataguba JE, Akazili J, Borghi J, Garshong B, et al. (2012) Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. The Lancet 380: 126-33.
- O'Donnell O (2007) Access to health care in developing countries: breaking down demand side barriers. Cadernos de saude publica 23: 2820-34.
- Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, et al. (2008) Poverty and access to health care in developing countries. Annals of the New York Academy of Sciences 1136: 161-71.
- Gluckman M, Liebow M, McLean RM, Musana KA, Nichols PM, et al. (2008) Achieving a high-performance health care system with universal access: what the United States can learn from other countries. Annals of internal medicine 148: 55-75.
- Starfield B (2012) Primary care: an increasingly important contributor to effectiveness, equity, and efficiency of health services 26: 20-26.
- Sehngelia L, Pavlova M, Groot W (2016) Impact of healthcare reform on universal coverage in Georgia: a systematic review. Diversity and Equality in Health and Care 13: 349-56.
- Ubel PA, Baron J, Nash B, Asch DA (2000) Are Preferences for Equity over Efficiency in Health Care Allocation "All or Nothing"? Medical Care 38: 366-73.
- Reidpath DD, Olafsdottir AE, Pokhrel S, Allotey P (2012) The fallacy of the equity-efficiency trade off: rethinking the efficient health system. BMC Public Health 12: 3.
- Culyer AJ (2015) Efficiency, equity and equality in health and health care. In: York Uo, editor. Center for Health Econ 1-20.
- Chalkidou K, Glassman A, Marten R, Vega J, Teerawattananon Y, et al. (2016) Priority-setting for achieving universal health coverage. Bulletin of the WHO 94: 462-467.
- Sabik LM, Lie RK (2008) Priority setting in health care: Lessons from the experiences of eight countries. Int J Equity in Health 7: 4.
- Mitton C, Donaldson C (2009) Priority setting toolkit: guide to the use of economics in healthcare decision making.
- Norheim OF, Baltussen R, Johri M, Chisholm D, Nord E, et al. (2014) Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Eff Resour Alloc 12: 18.
- Cookson R, Mirelman AJ, Griffin S, Asaria M, Dawkins B, et al. (2017) Using Cost-Effectiveness Analysis to Address Health Equity Concerns. Value in Health 20: 206-12.
- Johri M, Norheim OF (2012) can cost-effectiveness analysis integrate concerns for equity? Systematic review. Int J Technology Assessment in Health Care 28: 125-32.
- Norheim OF, Baltussen R, Johri M, Chisholm D, Nord E, et al. (2014)Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Effectiveness and Resource Allocation 12: 18.
- Norheim OF, Baltussen R, Johri M, Chisholm D, Nord E, et al. (2014) Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Eff Resour Alloc 12: 18.
- Mobinizadeh M, Raeissi P, Nasiripour AA, Olyaeemanesh A, Tabibi SJ (2016) The health systems' priority setting criteria for selecting health technologies: A systematic review of the current evidence. Med J Islam Repub Iran. 30: 329.
- Greco S, Figueira J, Ehrgott M (2016) Multiple criteria decision analysis.
- Kaplan RM, Babad YM (2011) Balancing influence between actors in healthcare decision making. BMC health services research 11: 85.
- Institute PHR (2009) The price of excess: identifying waste in healthcare spending.
- Thomson Reuters (2009) Where can $700 billion in waste be cut annually from the US healthcare system?.
- Berwick DM, Hackbarth AD (2012) Eliminating waste in US health care. Jama 307: 1513-1516.
- Singh A, Naik V, Lal S, Sengupta R, Saxena D, et al. (2011) Improving the efficiency of healthcare delivery system in underdeveloped rural areas. 2011 Third International Conference on Communication Systems and Networks (COMSNETS 2011) IEEE.
- Koppar AR, Sridhar V (2009) A workflow solution for electronic health records to improve healthcare delivery efficiency in rural india. 2009 International Conference on e Health, Telemedicine, and Social Medicine;: IEEE.
- Bhat VN (2005) Institutional arrangements and efficiency of health care delivery systems. European J Health Econ 6215-6222.
- Baum F, Freeman T, Sanders D, Labonte R, Lawless A, et al. (2016) Comprehensive primary health care under neo-liberalism in Australia. Social science & medicine (1982). 168: 43-52.
- Chambers D, Cantrell A, Johnson M, Preston L, Baxter SK, et al. (2019) Health Services and Delivery Research. Digital and online symptom checkers and assessment services for urgent care to inform a new digital platform: a systematic review. NIHR Journals Library.
- Banham D, Lynch J, Karnon J (2011) An equity-effectiveness framework linking health programs and healthy life expectancy. Australian J primary health 17: 309-19.
- Baeten SA, Baltussen RM, Uyl-de Groot CA, Bridges J, Niessen LW (2010) Incorporating equity-efficiency interactions in cost-effectiveness analysis-three approaches applied to breast cancer control. Value in health : J Int Society for Pharmacoeconomics and Outcomes Res 13: 573-9.
- Ahlert M, Schwettmann L (2017) Allocating health care resources: a questionnaire experiment on the predictive success of rules. Int J Equity Health 16: 112.
- Arbel R, Greenberg D (2016) Rethinking cost-effectiveness in the era of zero healthcare spending growth. Int J Equity Health 15: 33.
- Ashton T, Cumming J, Devlin N (2000) Priority-setting in New Zealand: translating principles into practice. J health services res policy 5: 170-5.
- Tromp N, Baltussen R (2012) Mapping of multiple criteria for priority setting of health interventions: an aid for decision makers. BMC health services research 12: 454.
- Cromwell I, Peacock SJ, Mitton C (2015 ) ‘Real-world’ health care priority setting using explicit decision criteria: a systematic review of the literature. BMC health services research 15: 164.
- Cafagna G, Seghieri C, Vainieri M, Nuti S (2018) A turnaround strategy: improving equity in order to achieve quality of care and financial sustainability in Italy. Int J equity in health 17: 169.
- Baltussen R, Mikkelsen E, Tromp N, Hurtig A, Byskov J, et al. (2013) Balancing efficiency, equity and feasibility of HIV treatment in South Africa–development of programmatic guidance. Cost effectiveness and resource allocation 11: 26.
- Arredondo A, Orozco E, Aviles R (2015) Evidence on equity, governance and financing after health care reform in Mexico: lessons for Latin American countries. Saúde e Sociedade 24: 162-75.
- Mirelman A, Mentzakis E, Kinter E, Paolucci F, Fordham R, et al. (2012) Decision-making criteria among national policymakers in five countries: a discrete choice experiment eliciting relative preferences for equity and efficiency. Value in health 15: 534-539.
- Arredondo A, Orozco E (2008) Equity, governance and financing after health care reform: lessons from Mexico. Int J health planning manag 23: 37-49.
- Sin DD, Svenson LW, Cowie RL, Man SP (2003) Can universal access to health care eliminate health inequities between children of poor and nonpoor families?: A case study of childhood asthma in Alberta. Chest 124: 51-56.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences