Principles of Soft Tissue Management in Dental Implants
Mao XQ
DOI10.21767/2471-9927.100027
Mao XQ*
Department of Implantology, Stomatology Center, Affiliated Haikou Hospital of Central South University, Xiangya Medical School, 43 Renmin avenue, Haikou 570208, China
- *Corresponding Author:
- Xiao-quan Mao
Department of Implantology, Stomatology Center
Affiliated Haikou Hospital of Central South University
Xiangya Medical School
43 Renmin Avenue, Haikou 570208, China
Tel: +86 0898-66189676
E-mail: horse.m@163.com
Received date: January 10, 2017; Accepted date: February 15, 2017; Published date: February 15, 2017
Citation: Mao XQ. Principles of Soft Tissue Management in Dental Implants. J Health Med Econ. 2017, 3:1. doi: 10.21767/2471-9927.100027
Abstract
Objective: To evaluate the impact of soft tissue factors in dental implants. Data: Studies evaluating the role of soft tissues in dental implants were included in this review.
Sources: A comprehensive literature search of English and Chinese language articles was performed via electronic databases (PubMed, Cochrane Library, Web of Science, CNKI and VIP) using the appropriate key words(esthetic; evaluation; impact factor; soft tissue). The most recent search took place in January 2016.
Study selection: Potentially appropriate articles were identified and evaluated for eligibility through a predefined review process conducted by two examiners. Only 16 out of the 346 identified records met criteria and were included in the final analysis.
Conclusion: The success of dental implants depends on two outcomes, the functional utility of the implant and its beauty. During the early phase of treatment, the main objective of a dental implant is to achieve adequate function. In clinical practice, however, subsequent soft tissue retraction and implant exposure have a significantly negative impact on implant esthetics, especially in young women's teeth, which can also be considered as implant failure. It is particularly important to understand how to support the surrounding soft tissue so that it is esthetically pleasing.
Keywords
Esthetic; Evaluation; Impact factor; Soft tissue
List of abbreviations used
BW: Biologic width; CPB: The distance between alveolar ridge crest to Crown Point of contact; KMW: Keratinized mucosa width
How does One Evaluate Soft Tissue Esthetics?
The Pink Esthetic Score (PES) is a simple yet complete tool for assessment of esthetic parameters [1]. The PES is a composite score of the tooth volume/outline [2], mesio-gingival papilla, distal gingival papilla, labial margin curvature, labial edge height, and the color and texture of soft tissue.
How does one categorize the gingival papilla level? Gingival papilla level 0: no gingival papilla; level 1: gingival papilla < ½ teeth gap; level II: gingival papilla > ½ teeth gap; level III: gingival papilla is full of teeth gap; level IV: gingival papilla overgrowth teeth gap.
The Impact Factors of Soft Tissue
Gingival biotype
Gingival biotype is the thickness of the gingiva in the faciopalatal dimension [3]. Generally, the biological types of gums are divided into 2 types: thin and thick gingival biotype. It is defined thick gingival biotype when the thickness of the buccal mucosa is larger than or equal to 1.5 mm. It is defined thin gingival biotype when the thickness of the buccal mucosa is less than 1.5 mm. Probe visibility is the clinical gold standard to discriminate thick biotypes from thin ones, but this method is prone to subjective interpretation. It has a significant impact on the outcome of restorative, regenerative implant therapy. Biotype is one of the critical factors that determine the result of dental treatment. Initial gingival thickness predicts the outcome of any root coverage procedures or any restorative treatments. Compared with thin gingival biotype, thick ones have obvious advantages in preventing the withdrawal of fibrous tissue and bone tissue [4], besides the support of more blood supply.
Biologic width (BW)
The distance between supracrestal soft tissue attachment of periodontal tissue and the tooth/root surface has been termed biologic width [5], an important concept in periodontics and restorative dentistry. Both attached epithelial cells and connective tissue attachment complex make important contributions to periodontal health during prosthetic treatments, since invading this zone can cause bone resorption and gingival recession. The concept is introduced into the field of implantation. Implant biologic width is the distance established by "the junctional epithelium and connective tissue attachment to the implant surface". In other words, it is the height between the deepest point of the gingival sulcus and the alveolar bone crest. This kind of natural enclosure can provide isolation from the oral environment and protection for peri-implant bone tissue in order to maintain the stability of implants. The mean biologic width was determined to be 2.04 mm, of which 1.07 mm is occupied by the connective tissue attachment and another approximate 0.97 mm is occupied by the junctional epithelium [6,7].
The relationship between biotype and biologic width: The thicker biotype of the gingival mucosa has the more enough space to support biologic width. In other words, during dental restoration in a patient with thick biotype gingival mucosa, it is more difficult to infringe upon the biologic width. An esthetic outcome is much more likely gained in thick biotype gingival mucosa.
Thickness of labial bone wall
Esthetic effect obtained in the labial gingiva [8] is closely related to labial lateral bone wall thickness. Thickness greater than 2mm gives greater certainty of aesthetic effect and implant stability.
Distance between implants
The long-term success [9] of restorative implants is based upon the biology and vasculature of bone surrounding the implants, especially the bone between two implants. The ideal lateral space between implants and tooth is 3-4 mm. Gastaldo [10] found that it is difficult to form gingival papilla when the distance between implant edges or the horizontal distance between adjacent teeth is less than 3 mm. The inter-implant distance should not be less than 3 mm and the distance between the natural teeth and implants should be at least 1.5 mm in order to ensure that the peri-implant is surrounded by the integrity of alveolar bone.
Distance between Crown contact point-alveolar bones (CPB)
CPB [11] is the distance between the crowns of the teeth to the crest of bone. CPB less than or equal to 5 mm results in an ideal esthetic effect. If CPB is less than or equal to 4 mm, gingival papilla recovery is 100%; if CPB is greater than 4 mm but less than or equal to 5 mm, average gingival papilla recovery is up to 88%; if CPB is greater than 5 mm, gingival papilla recovery is less than 50%. In addition, some scholars believe that in maxillary anterior teeth area single tooth implant restoration, controlling CPB to less than or equal to 4 mm, can avoid the "black triangle".
Relationship between the distance of implants and CPB: A wider distance between implants corresponds with a lower CPB, the teeth gap can be filled with gingival papilla more easily. In other words, when considering the distance between implants, one should take into account the CPB. Otherwise, it may be difficult to fill the gap between the dental implants and therefore difficult to guarantee an esthetic outcome.
Keratinized mucosa width (KMW)
Keratinized gums around the natural tooth and implant play several important roles, including: withstanding mechanical friction and avulsion, counteracting adjacent tension of the fraenum linguae, stabilizing the gingival margin, preventing plaque retention and buffering the biological forces from the mucous membrane of muscle fibers. Therefore, the contribution of a proper Keratinized mucosa width is to maintain the healthy defense mechanism of tissues surrounding the implants. Lang’s [12] study of the relationship between gingival and periodontal health proposed that in order to maintain healthy gums, one must have a 2mm wide keratinized gum, including 1 mm of free gingiva and 1 mm of attached gingiva. When KMW was greater than 2 mm, there was no detectable plaque or gum inflammation on the tooth surface. When KMW was less than 2 mm, there was obvious gingival recession. This positive effect of the gums surrounding the implant leads to a considerably better esthetic effect.
Condition of adjacent teeth
Periodontitis in adjacent teeth can affect esthetics [13], whereby resulting in alveolar bone resorption, which may lead to reduced or absent papilla between implants. In addition, implant failure may occur due to coexistent inflammation in the root apex, which can affect the adjacent bone tissue within 1 cm of the root apex [14,15].
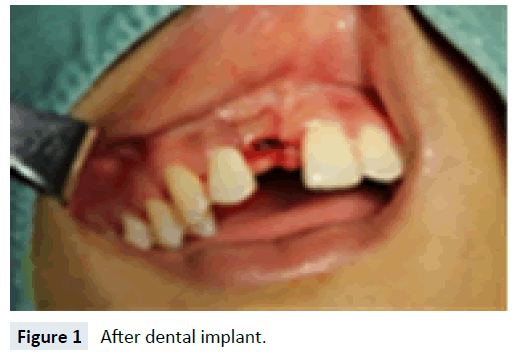
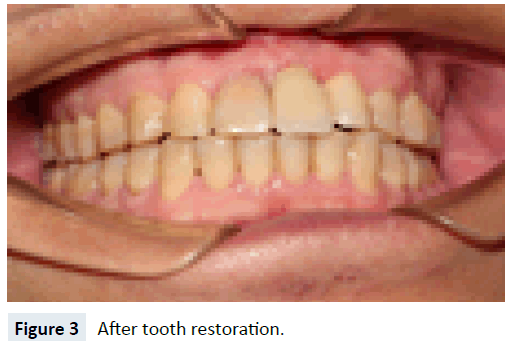
Suture
The role of surgical suture is to maintain tension in the wounds and promote the healing. Ideally, sutures should have a certain tensile strength and a stable absorption rate, while at the same time provoking only a mild histologic reaction and demonstrating predictable in vitro performance (Figures 1-3).
Discussion
Dental Implants [16] are today considered as a reliable treatment option to replace missing teeth both for esthetics and function. The success of an implant restoration depends on proper implant placement and the hard and soft tissue architecture that surrounds the fixture and its gums, shape, color and texture is coordinated with adjacent teeth that close to the state of the nature. The gingival papilla exists or not and its shape are important factors that effect on the aesthetic of implant denture, but it has certain limitations to recover the loss of gingival papilla and easy to be ignored, so the implant denture gingival papilla aesthetic problems have gradually become the current focus of the field of dental implants.
The aesthetic effect of the gingival papilla is still the bottleneck in implant denture restoration at present, but the aesthetic effect can be predicted according to anatomy of adjacent edentulous space, it is conducive for the physicians and patients to choose treatment scheme in order to achieve aesthetic and functional results. In addition, healthy keratinized gingiva is an important factor to ensure the aesthetic effect of dental implant restoration, especially in the anterior and premolar area.
In order to obtain long-term stable aesthetic restoration, ensure the health of soft tissue and coordinate with the surrounding tissue, the transplantation of soft tissue technology, appropriate healing cap and a temporary soft tissue remodeling can be used when soft tissue is not adequate. The reconstruction of the soft tissue surround the implant denture is to provide a stability of the gingival structure. Because stable soft tissue surround the implant denture can provide a close and mechanical defence to prevent bacterial invasion and improve long-term success rate.
In order to obtain satisfactory and aesthetic restoration, we should improve the implantation plan to repair the factors that affect the aesthetics of the implant denture by layer analysis and processing.
References
- Perelli M, Abundo R, Corrente G, Saccone C, Zambelli M (2015) Implant-supported prostheses esthetic outcomes after socket preservation technique. Journal of Craniofacial Surgery 26: 729-30.
- Hae-Lyung Cho, Jae-Kwan Lee, Heung-Sik Um, Beom-Seok Chang (2010) Esthetic evaluation of maxillary single-tooth implants in the esthetic zone. Journal of Periodontal & Implant Science 40: 188-193.
- Manjunath RG, Rana A, Sarkar A. (2015) Gingival Biotype Assessment in a Healthy Periodontium: Transgingival Probing Method. Journal of Clinical & Diagnostic Research 9: ZC66-9.
- Frost NA, Mealey BL, Jones AA, Huynh-Ba G (2015) Periodontal Biotype: Gingival Thickness as it Relates to Probe Visibility and Buccal Plate Thickness. Journal of Periodontology 86: 1141-1149
- Rasouli Ghahroudi AA, Khorsand A, Yaghobee S, Haghighati F (2014) Is biologic width of anterior and posterior teeth similar? Acta Medica Iranica 52: 697-702.
- Cochran DL, Obrecht M, Weber K, Dard M, Bosshardt D, Higginbottom FL, et al. (2014) Biologic width adjacent to loaded implants with machined and rough collars in the dog. International Journal of Periodontics & Restorative Dentistry 34: 773-9.
- Reetika Gaddale, Jayashree Mudda, Ilangovan Karthikeyan, Shrikar Desai, Harshada Hemchandra Shinde, et al. (2015) Determination of clinical biologic width in chronic generalized periodontitis and healthy periodontium: A clinico-radiographical study. Journal of Indian Society of Periodontology19: 194-198.
- Yang Guang, Yan Minmin (2013) Clinical observation and operation designs of implant surgery in cases of maxillary central incisor lost with insufficient alveolar bone. Stomatology 33: 245-247
- Traini T1, Novaes AB, Piattelli A, Papalexiou V, Muglia VA (2010) The relationship between interimplant distances and vascularization of the interimplant bone. Clinical Oral Implants Research 21: 822-829.
- Gastaldo JF, Cury PR, Sendyk WR (2004) Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. Journal of Periodontology 75: 1242-1246.
- Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP, et al. (2001) Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. Journal of Periodontology 72: 1364-1371.
- Lang NP, Loe H (1972) The relationship between the width of keratinized gingiva and gingival health. Journal of Periodontology 43: 623-627
- Zhan Fuliang, Liu Ce, Liu Xianghua (2013) The vital tooth lesions lead to chronic maxillary sinusitis in 3 cases. China Practical Journal of Department of Stomatology 6: 766-768
- Cheng Yanan, Xu Pu, Jian Xinchun, Lu Liying, Zheng Tongwen, et al. (2013) Implant failure for retrograde peri-implantitis. Chinese Journal of Stomatology 48: 383-384
- Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M (2011) Cone-beam computed tomography evaluation of maxillary sinusitis.Journal of Endodontics 37:753-757.
- Vaibhav Joshi, Shalini Gupta (2015) Immediate Implant Placement in Anterior Aesthetic Region and Assessment using Cone-Beam Computed Tomography Scan Technology. J Int Oral Health 7: 99-102.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences